The Swoop® system
Putting AI-powered portable MRI in your hands

TRANSFORMING BRAIN IMAGING
BRINGING MRI TO MORE PEOPLE IN MORE PLACES AROUND THE WORLD
The Swoop system is an AI-powered, portable brain MRI that uses a magnet with a fraction of the field strength used in conventional MRI. This means it can be brought to the point of care and used safely in almost any care setting without the need for dedicated staff or infrastructure.
PRODUCT IMAGES AND VIDEOS



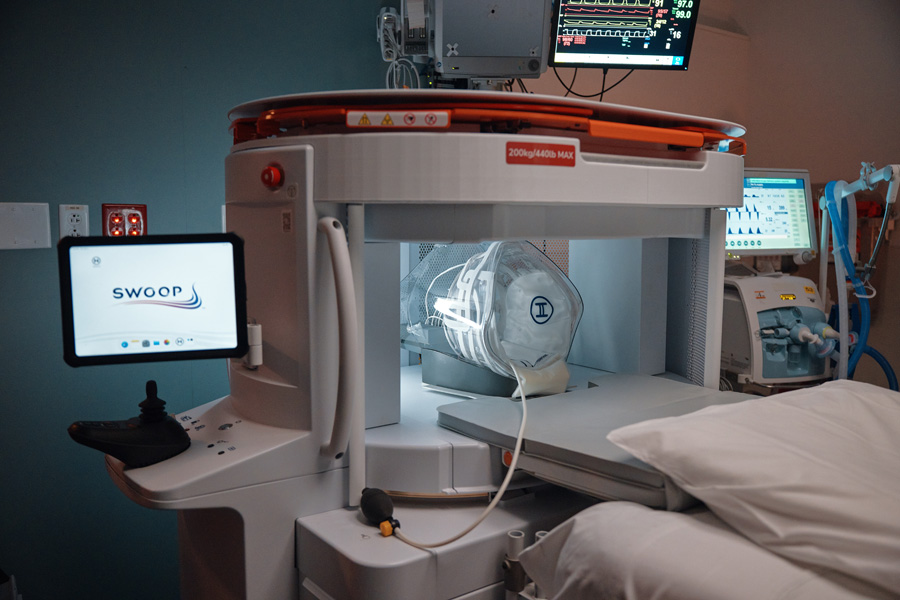







The Swoop System Powered By

Powering the Future of Portable MRI
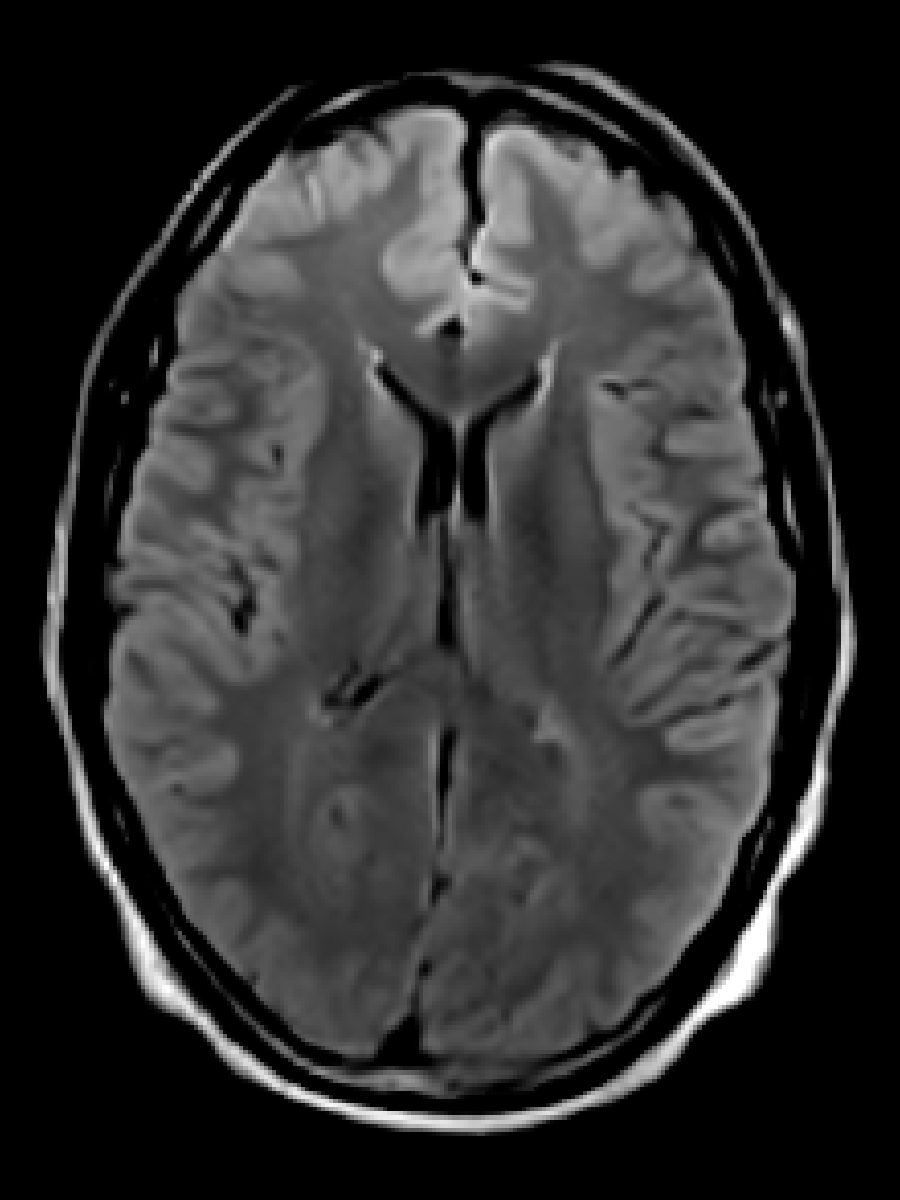
Optive AI™ software brings advanced, AI-driven image reconstruction to ultra-low-field (0.064T), portable MRI—unlocking clearer images at lower field strengths.
By reducing noise and blur with deep learning, it enhances image clarity and consistency, providing sharper anatomical detail to support confident diagnoses at the point of care.
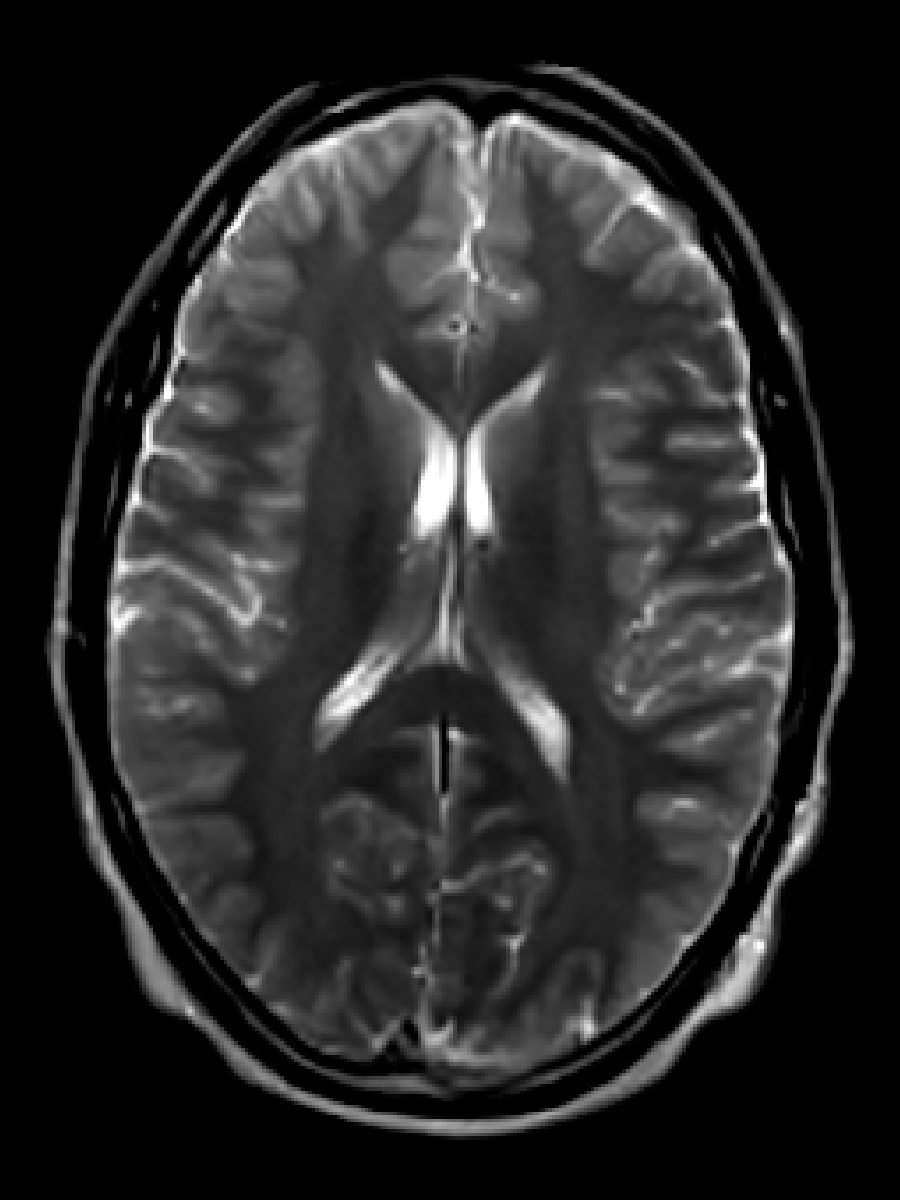
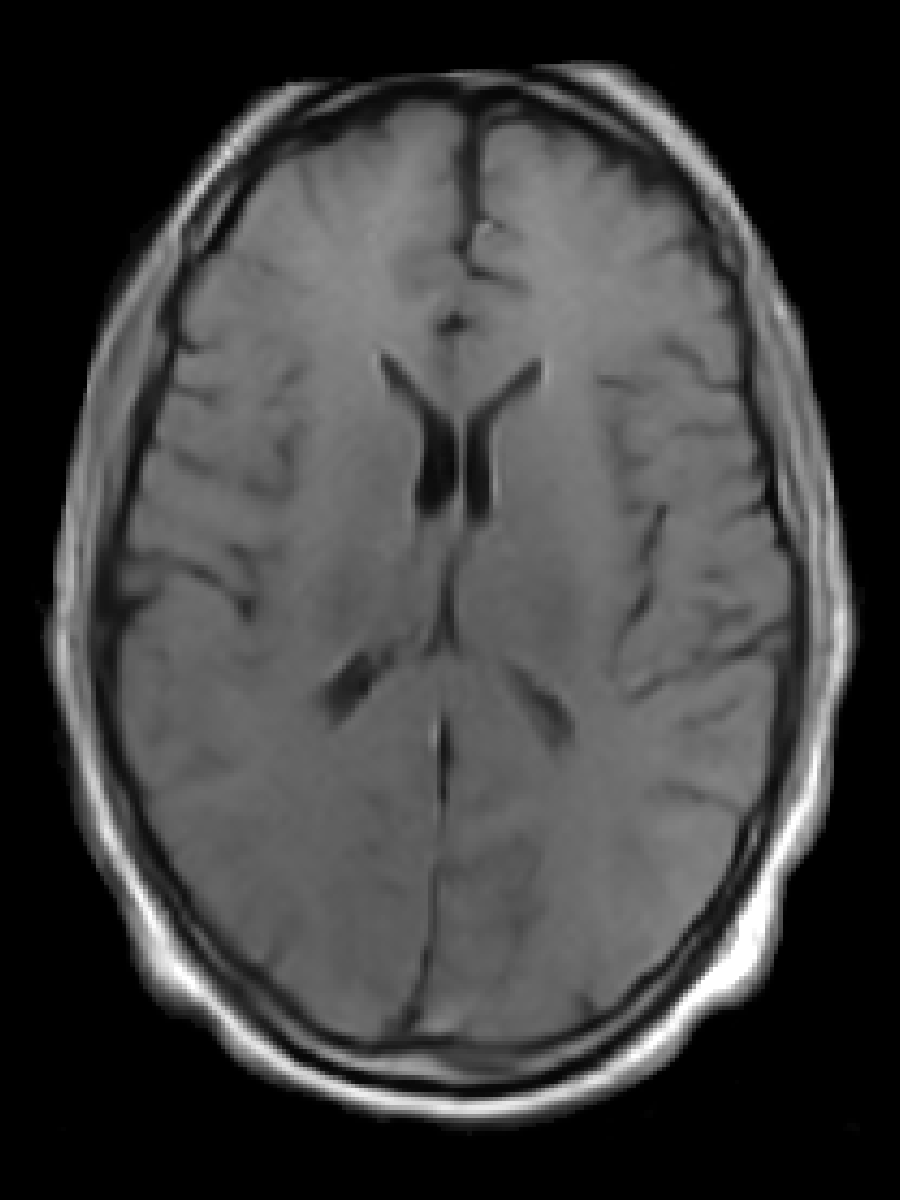
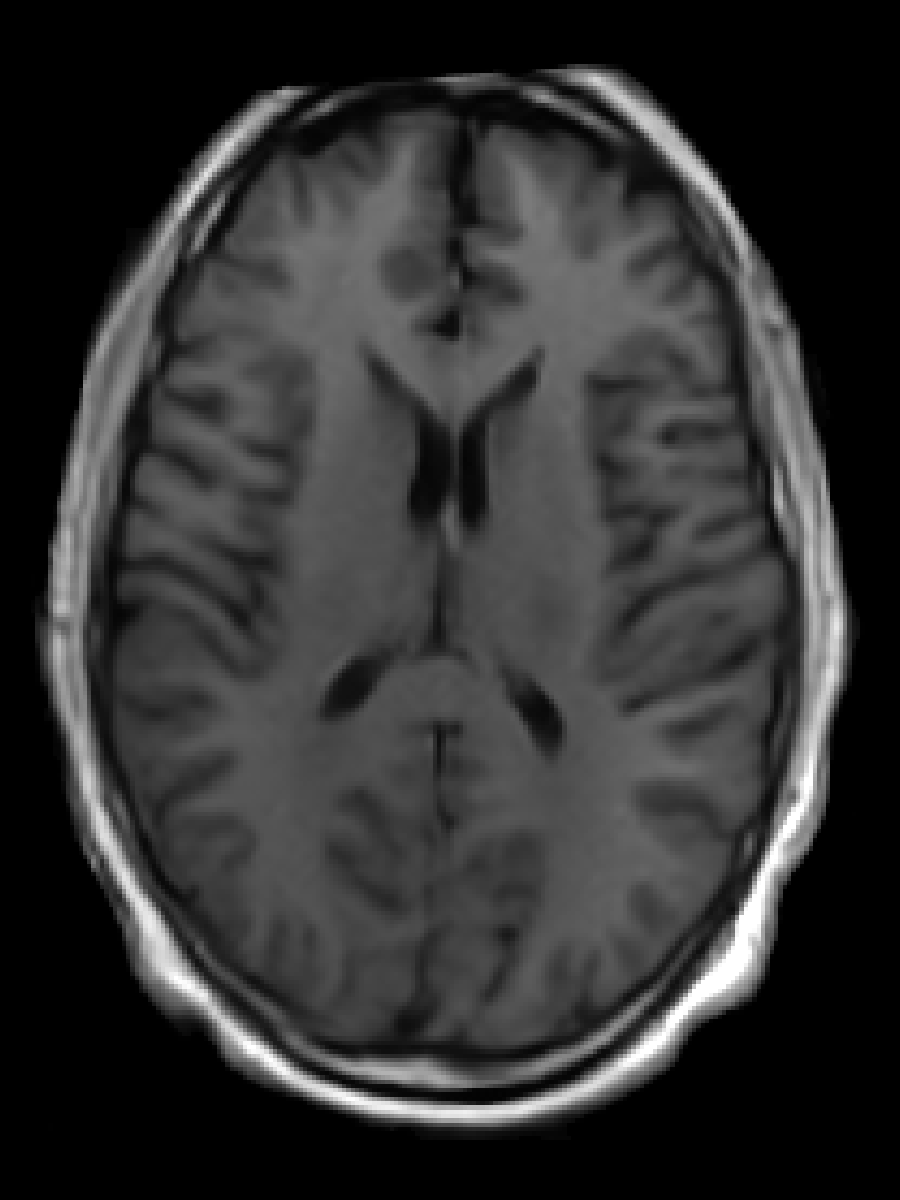
Swoop System Sequence Images
Sequences include T1 (Standard), T1 (Gray/White), T2, Fast T2, FLAIR, Fast FLAIR, DWI with ADC, and Fast DWI with ADC. The T1, T2, and FLAIR sequences are available in the axial, coronal, and sagittal planes.
THE SWOOP SYSTEM IN YOUR HANDS
Healthcare professionals in almost any clinical setting can now be empowered with advanced imaging capability.

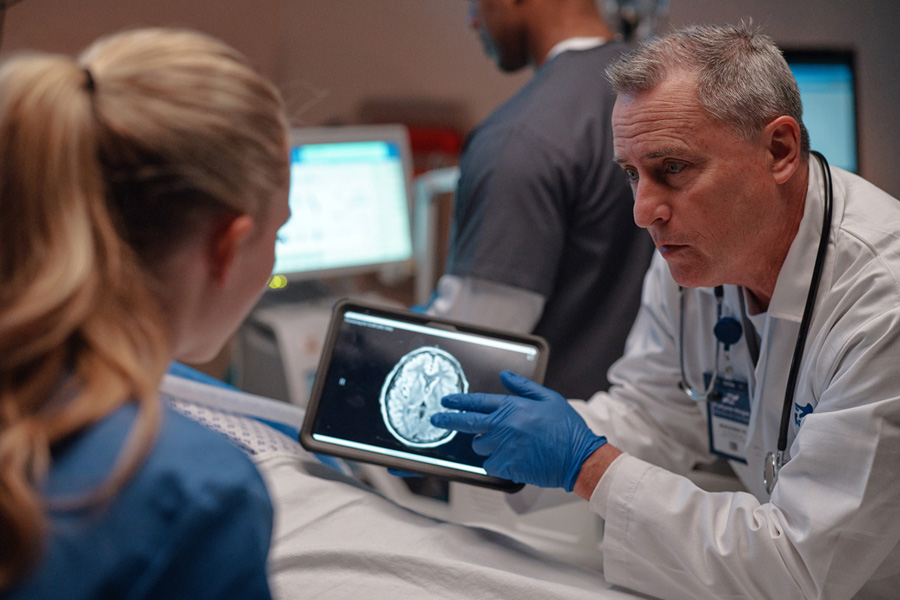
In The Hospital
The Swoop system can empower healthcare professionals to make informed decisions and deliver prompt, cost-effective care in both the ICU and high-pressure emergency department settings.

In Neurology Clinics
The Swoop system provides brain imaging directly in your exam room. Best of all, it's cost-effective, easy to implement, and eligible for reimbursement, making it a smart investment for comprehensive neurology practices.

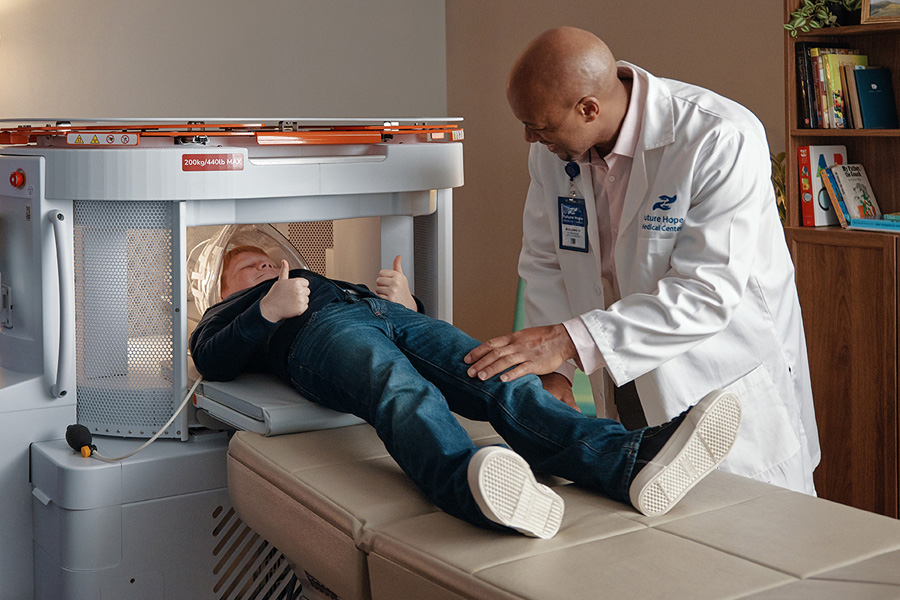
In Pediatrics
The Swoop system makes scans less scary with a quiet, open design and no exposure to ionizing radiation. Best of all, parents can stay right next to their child the entire time.