AI-Powered Portable MRI for Pediatric Patients







Making Medical Imaging Safer and
More Comfortable for Kids

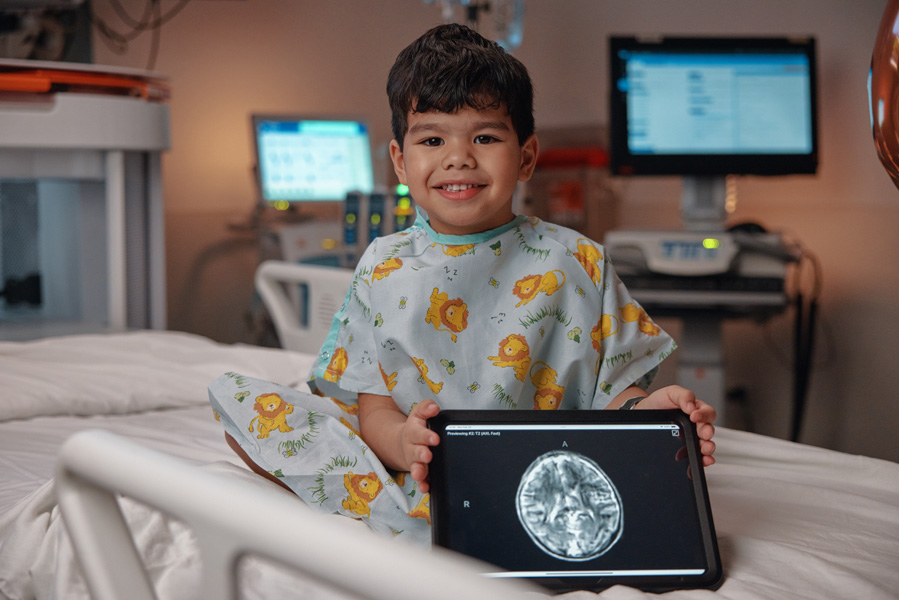
A Child-Friendly Imaging Solution
The Swoop® system offers a child-friendly imaging solution designed to minimize distress and discomfort while providing valuable diagnostic imaging—all without exposing children to ionizing radiation.

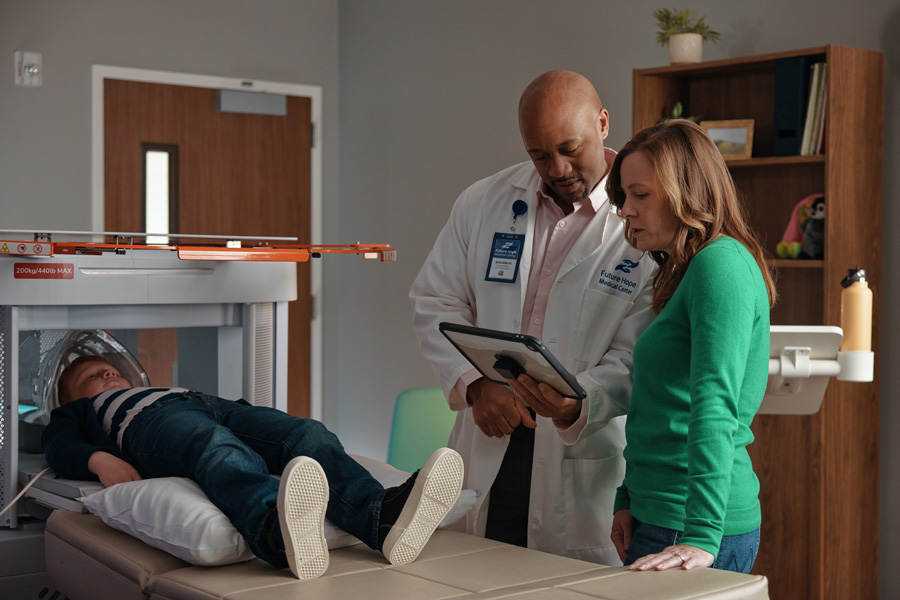
Facilitates Moments of Comfort and Care
Parents can remain at their child’s side
Parents can remain at their child’s side and hold their hand during the scan, providing comfort and reassurance throughout the experience.
Allows comfort items
Allows comfort items such as stuffed animals and pacifiers to help children stay relaxed.

Designed to Ease Anxiety
Open design
Open design for a less claustrophobic experience.
Substantially quieter operation
Substantially quieter operation eliminates the need for hearing protection and provides a less intimidating scan.
Advancing Pediatric Care Across Settings
The Swoop system provides valuable imaging in neurosurgery clinics, the pediatric ICU, and the emergency department.

Clinicians may find the Swoop system useful for assessing children with:
- Hydrocephalus (diagnosis and monitoring)
- Post-operative assessment needs
- Metal accessories, including braces
- Suspected stroke
- Suspected abuse
- Acute mental status change
Avoids Exposure to Harmful Radiation
Unlike CT, Swoop system scans are free of ionizing radiation, making it a safer alternative for children, especially those needing repeat imaging, such as hydrocephalus patients.
