Radiology, portable MR brain imaging, and ICU patients.
Summary
- Conventional high-field MRI scans for acute and critical care patients pose significant logistical challenges, patient transport risks, and increase stress on hospital staff and resources.
- The Swoop system brings brain imaging to critically ill patients in the ICU, avoiding intrahospital transport risks and allowing uninterrupted ICU monitoring.
- The Swoop system potentially enhances ICU efficiency by minimizing staff coordination for patient transport and delivering brain imaging hours sooner than conventional MRI.
The challenges with imaging ICU patients using conventional high-field MRI systems.
Since its inception, magnetic resonance imaging (MRI) has assumed an increasingly important role in the clinical management of patients with neurologic disorders. With the development of diffusion-weighted and susceptibility-weighted sequences, MR neuroimaging has become important in acute and hyperacute situations. In practice, clinicians must weigh the benefits of these sequences against the challenges of imaging patients with such acute conditions
Nearly every hospital faces the challenge of transporting neurocritical patients for MR imaging. Some have tried installing MRI systems near the point of care. On the resource side, a conventional MRI system near an ICU needs a dedicated space for the standard shielded area, reinforced physical structures, and an MR safe zone (a safety standard expected as part of MR accreditation). With enough resources these structural issues are solvable. However, even when a system is located near the point of care, patients must still be transported to the MRI system along with specialized MR-compatible equipment.
For the majority of hospitals, the only viable option is to transport critical patients to a radiology suite located some distance from the ICU in another area of the facility. Many radiologists and physicians are not exposed to the complexities required of ICU nurses and respiratory therapists to bundle and safely transport patients in such a complex state. The issue isn’t the scan time—it’s the time required for patient preparation and transport, MRI availability (scheduling, wait time in the anteroom or hallway, etcetera), and the potential for adverse events during transport.

Even under the supervision of a well-trained transport team, adverse events may still occur in 26–79% of cases during transport to imaging1,2,3,4. Difficulties occur with hardware, challenges with lifts to move the patient, issues with infusion lines, and limited battery life for equipment needed to support the patient5. Moreover, the problems around scanning critically ill patients are complicated by stress on the hospital staff. By removing nurses and therapists to facilitate patient transport to radiology, the ICU has fewer staff members to care for the other critical patients.
Despite recent advances using compressive sensing to shorten MRI scan times, studies have demonstrated that the overall turnaround time from order to actionable results for ICU patients is anything but short. According to Glavis et al., the workflow for imaging an ICU patient with conventional high-field MRI can take as long as 11.7 hours6 at their hospital. Other hospitals have anecdotally reported up to 24 hours.

The complexities of the traditional workflow for neuroimaging of critical patients take a toll on everyone involved, from the risk to the patient to the stress and increased workload for the entire ICU staff. What if transport-related adverse events and the resulting impact on the quality of care were not part of the equation? What if clinicians could neuroimage patients who were too ill for transport? What if specialized nurses could stay in the ICU with the patient—where they can take better care of the patient?
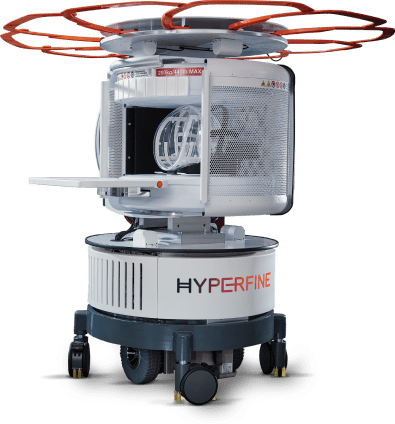
The Swoop® system—the Hyperfine, Inc. solution.
By bringing diagnostic MR imaging to the point of care, a Swoop® Portable MR Imaging® system may potentially prevent adverse events related to transport and reduce patient care interruptions. The Swoop system may also contribute to reducing the length of stay (and associated costs) in the ICU by enabling clinical care teams with the potential to optimize staffing and shorten the time to diagnosis. And, it’s not just the length of stay of the ICU patients—by scanning ICU patients with the Swoop system, other inpatients may be scanned earlier, no longer having to wait for the ICU patients to be scanned.


In addition to the many patient and clinician benefits, the Swoop system costs a fraction of the capital investment required for a high-field MRI system and doesn’t require helium or additional electrical and structural infrastructure. Moreover, deploying a Swoop system incurs no siting costs, typically $1M or more for conventional MRI systems. The Swoop portable MR brain imaging system is complementary to conventional high-field MR imaging systems, offering simple operation, navigation, and safety training, which allows for expanded user, operator, and patient access.
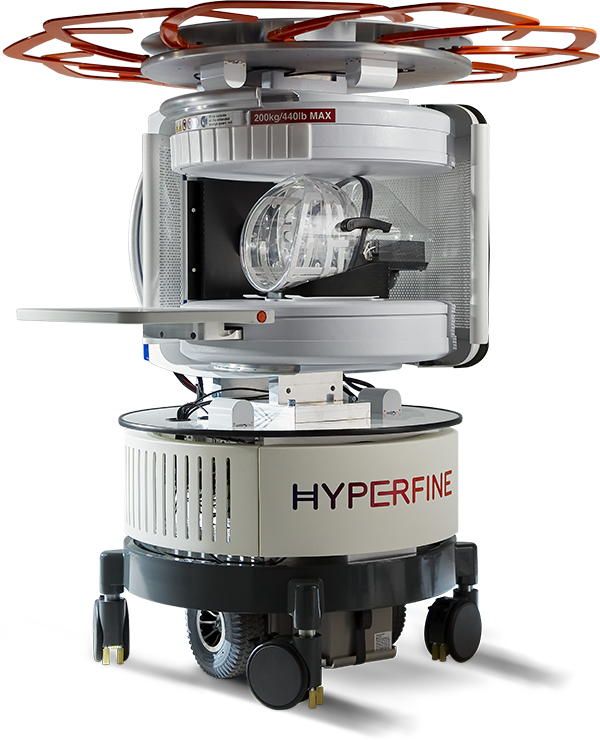
For the patient, the Swoop system reduces potential adverse events associated with patient transport and brings neuroimaging to the bedside of critically ill patients who are too unstable for transport to radiology. The Swoop system complies with EMC emission standards and is not expected to affect most ICU equipment. Patients can remain connected to all intravenous lines and most ICU monitoring equipment as long as it remains outside the controlled access area.
For the hospital, a Swoop system can help optimize staffing in the ICU by reducing the time required to coordinate clinical schedules and support staff for patient transport to radiology, allowing caregivers to remain where they’re needed most—in the ICU at the patient’s bedside or available to assist other patients. In addition to optimizing staff time, with a Swoop system in an ICU, images can be available three to seven hours earlier than those from conventional MRI.
Additionally, a Swoop system enables clinicians to monitor a patient’s condition at the point of care, providing clinicians with real-time information to assist in critical care management decisions—without patient transport (and its associated risks) and without subjecting patients and staff to ionizing radiation from the portable CTs often used for serial follow-up scans.
In summary, the Swoop portable MR brain imaging system is a valuable clinical tool with the potential to improve neurocritical care workflows and patient outcomes by increasing access to neuroimaging and avoiding cumbersome patient transport to conventional MRI systems. Additionally, the Swoop system offers the potential for reduced length of stay for patients, improved staff utilization and quality of care, and less stress for both patients and care providers.
The Swoop® system is indicated for use as a portable, ultra-low field magnetic resonance imaging device for producing images that display the internal structure of the head where full diagnostic examination is not clinically practical. When interpreted by a trained physician, these images provide information that can be useful in determining a diagnosis.
Studies show that the Swoop system can provide images at the point of care that clinicians have found useful for assessing:
- Change in patient symptoms with an unknown cause—looking for new bleeds, mass effect, extra-axial collection, etcetera6,7,8,9
- Follow-up scans for clinically suspected or known strokes greater than 5mm10
- Change in ventricular size with or without intervention8,11
- Change in an intraparenchymal hematoma10
- Change in extra-axial collection11
- Change in the imaging appearance of infarct6
- To follow or confirm stability12
- Mass effect and potential for midline shift13
- Change post-thrombectomy14
The Swoop system in intensive care units.
Learn More
1. Jia L, Wang H, Gao Y, Liu H, Yu K. High incidence of adverse events during intra-hospital transport of critically ill patients and new related risk factors: a prospective, multicenter study in China. Crit Care. 2016;20:12. Published 2016 Jan 18. doi:10.1186/s13054-016-1183-y
2. Smith I, Fleming S, Cernaianu A. Mishaps during transport from the intensive care unit. Crit Care Med. 1990;18(3):278-281. doi:10.1097/00003246-199003000-00006
3. Martin M, Cook F, Lobo D, et al. Secondary Insults and Adverse Events During Intrahospital Transport of Severe Traumatic Brain-Injured Patients. Neurocrit Care. 2017;26(1):87-95. doi:10.1007/s12028-016-0291-5
4. Parmentier-Decrucq E, Poissy J, Favory R, et al. Adverse events during intrahospital transport of critically ill patients: incidence and risk factors. Ann Intensive Care. 2013;3(1):10. Published 2013 Apr 12. doi:10.1186/2110-5820-3-10
5. Beckmann U, Gillies DM, Berenholtz SM, Wu AW, Pronovost P. Incidents relating to the intra-hospital transfer of critically ill patients. An analysis of the reports submitted to the Australian Incident Monitoring Study in Intensive Care. Intensive Care Med. 2004;30(8):1579-1585. doi:10.1007/s00134-004-2177-9
6. Kuoy E, Glavis-Bloom J, Hovis G, et al. Point-of-Care Brain MRI: Preliminary Results from a Single-Center Retrospective Study [published online ahead of print, 2022 Aug 2]. Radiology. 2022;211721. doi:10.1148/radiol.211721
7. Sheth KN, Mazurek MH, Yuen MM, et al. Assessment of Brain Injury Using Portable, Low-Field Magnetic Resonance Imaging at the Bedside of Critically Ill Patients [published online ahead of print, 2020 Sep 8]. JAMA Neurol. 2020;78(1):41-47. doi:10.1001/jamaneurol.2020.3263
8. Beekman R, Crawford A, Mazurek MH, et al. Bedside monitoring of hypoxic ischemic brain injury using low-field, portable brain magnetic resonance imaging after cardiac arrest. Resuscitation. 2022;176:150-158. doi:10.1016/j.resuscitation.2022.05.002
9. Turpin J, Unadkat P, Thomas J, et al. Portable Magnetic Resonance Imaging for ICU Patients. Crit Care Explor. 2020;2(12):e0306. Published 2020 Dec 21. doi:10.1097/CCE.0000000000000306
10. Mazurek MH, Cahn BA, Yuen MM, et al. Portable, bedside, low-field magnetic resonance imaging for evaluation of intracerebral hemorrhage. Nat Commun. 2021;12(1):5119. Published 2021 Aug 25. doi:10.1038/s41467-021-25441-6
11. Sien ME, Robinson AL, Hu HH, et al. Feasibility of and experience using a portable MRI scanner in the neonatal intensive care unit [published online ahead of print, 2022 Jul 4]. Arch Dis Child Fetal Neonatal Ed. 2022;fetalneonatal-2022-324200. doi:10.1136/archdischild-2022-324200
12. Yuen MM, Prabhat AM, Mazurek MH, et al. Portable, low-field magnetic resonance imaging enables highly accessible and dynamic bedside evaluation of ischemic stroke. Sci Adv. 2022;8(16):eabm3952. doi:10.1126/sciadv.abm3952
13. Sheth KN, Yuen MM, Mazurek MH, et al. Bedside detection of intracranial midline shift using portable magnetic resonance imaging. Sci Rep. 2022;12(1):67. Published 2022 Jan 7. doi:10.1038/s41598-021-03892-7
14. Sujijantarat N, Koo AB, Jambor I, et al. Low‐Field Portable Magnetic Resonance Imaging for Post‐Thrombectomy Assessment of Ongoing Brain Injury. Stroke. 2023;3:e000921. Published 2023 Jul 24. doi:10.1161/SVIN.123.000921
The Swoop® system brings MR brain imaging within reach.
The Swoop system brings brain imaging within reach for clinicians to help them make clinical decisions in a variety of healthcare settings across a range of conditions. The first FDA-cleared portable MR brain imaging system that combines safe, ultra-low-field magnetic resonance with proprietary artificial intelligence, the Swoop system potentially enables timelier treatment decisions, quicker discharges, and more efficient use of staff and hospital resources.

