An executive perspective on portable MR brain imaging.
Summary
- Conventional MR imaging presents staffing, safety, and financial challenges. It requires complex patient transport for critically ill patients, which can jeopardize care quality and inflate hospital costs.
- The Swoop system brings brain imaging to critically ill patients in the ICU, avoiding intrahospital transport risks and allowing uninterrupted ICU monitoring.
- The Swoop system provides clinicians with portable and efficient bedside diagnostic brain imaging capabilities, potentially accelerating the diagnostic workflow and reducing ICU length of stay and healthcare costs.
Staffing, financial, and patient safety challenges with conventional MR neuroimaging.
Providing patients with the care they need and deserve while managing staffing and decreasing expenses is any healthcare facility’s primary focus. However, balancing these objectives is challenging when performing neuroimaging for critical patients. The traditional workflow for MR neuroimaging of critical patients requires intrahospital transport to an MR suite. Transport of critical patients is shown to significantly increase the risk of adverse events for patients, which has the potential to negatively and significantly impact quality of care and hospital expenses.

One of the most challenging aspects of transporting a patient is coordinating a specialized team to manage the patient as they move from the ICU to the MRI. Such a team typically includes two to six staff members. Further aggravating the situation, if the department is already short-staffed, taking staff away from the ICU to assist in imaging a patient could put other patients at risk. Additionally, each patient transport for imaging complicates the ICU workload, creating time-intensive patient care interruptions that require specialized nurses to remove and reattach life-sustaining equipment.
The risks and costs are well documented. According to Glavis et al., the workflow for imaging an ICU patient with conventional high-field MRI can take as long as 11.71 hours at their hospital. Other hospitals have anecdotally reported up to 24 hours. Additionally, intrahospital transport of patients is associated with numerous cardiovascular and respiratory risks that may limit timely and safe neuroimaging for critically ill patients2. Unfortunately, even under the supervision of a well-trained transport team, adverse events may still occur in 26–79% of cases during transport to imaging3,4,5,6.
Martin et al. reported that ventilator asynchrony was the most frequent adverse event and put patients at a higher risk for pneumothorax, atelectasis, and ventilator-associated pneumonia5. Difficulties occur with hardware, challenges with lifts to move the patient, issues with infusion lines, and a lack of battery life for equipment needed to support the patient7. In addition to patient impact, expenses are associated with each adverse event. According to a study by Mello et al., the average hospital-borne cost of an adverse event is $6,255 (adjusted for inflation)8.

The complexities of the traditional workflow for neuroimaging of critical patients take a toll on everyone involved, from the risk to the patient to the stress and increased workload for the entire ICU staff (not to mention the impact on a hospital’s bottom line). What if specialized nurses could stay in the ICU with the patient—where they can take better care of the patient while maximizing the nurse-to-patient ratio in the ICU? What if neuroimaging workflow for critical patients could be more effective and efficient? What if transport-related adverse event risks and the resulting impact on length of stay and hospital expenses were not part of the equation?
The Swoop® system—the Hyperfine, Inc. solution.
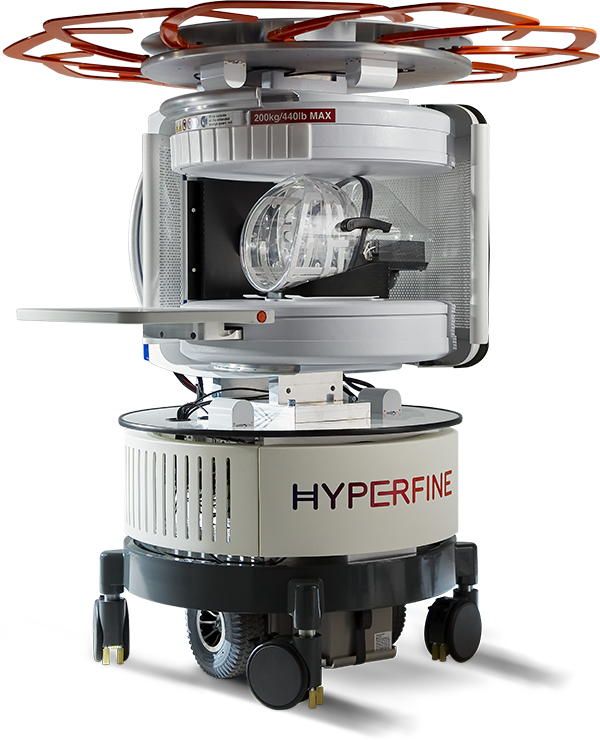
The Swoop® Portable MR Imaging® system enables operational efficiencies by reducing the need for intrahospital transports. Not every patient has to be transported to an MR suite when the Swoop system can bring MRI to the point of care. By bringing diagnostic MR imaging to the point of care, a Swoop system may potentially prevent adverse events related to transport and reduce patient care interruptions. The Swoop system may also contribute to reducing the length of stay (and associated costs) in the ICU by enabling clinical care teams with the potential to optimize staffing, expedite and improve patient care, and shorten the time to diagnosis. Point-of-care MR imaging can take as little as 0.5 to 5.3 hours, from ordering the scan until the images are available for assessment—a significant time reduction from the 11.7 hours it takes for conventional high-field MR imaging of critical patients.
In addition to the many benefits for patients and clinicians, the Swoop system is more cost-effective to own and maintain than conventional high-field MRI systems. Unlike conventional high-field MRI, which requires specialized infrastructure and radiologic technicians, Swoop system operation, navigation, and safety training are simple, allowing for expanded user access.

For the patient, the Swoop system reduces potential adverse events associated with patient transport and brings neuroimaging to the bedside of critically ill patients who are too unstable for transport to radiology. The Swoop system complies with EMC emission standards and is not expected to affect most ICU equipment. Because of this, patients can remain connected to all intravenous lines and most ICU monitoring equipment as long as it remains outside the 62-inch diameter controlled access area.
For the hospital, using a Swoop system in an ICU can help optimize scheduling and increase efficiency in ICU staff utilization by reducing the time required to coordinate patient transport to radiology. Also, ICU staff can remain where they’re most needed—in the ICU at the patient’s bedside or available to assist other patients.
Additionally, a Swoop system enables clinicians to image a neuro critical care patient at the point of care, providing clinicians with real-time information to assist in critical care management decisions—without patient transport (and associated risks and costs) and without subjecting patients and staff to ionizing radiation from the portable CTs often used for serial follow-up scans.
With a Swoop portable MR brain imaging system in an ICU, hospitals have the potential to establish a new standard of care for patients too ill to transport while supporting long-term organizational goals and focusing on the best care for patients.
The Swoop® is indicated for use as a portable, ultra-low field magnetic resonance imaging device for producing images that display the internal structure of the head where full diagnostic examination is not clinically practical. When interpreted by a trained physician, these images provide information that can be useful in determining a diagnosis.
Studies show that the Swoop system can provide images at the point of care that clinicians have found useful for assessing:
- Change in patient symptoms with an unknown cause—looking for new bleeds, mass effect, extra-axial collection, etcetera2,9,10,11
- Follow-up scans for clinically suspected or known strokes greater than > 5mm9
- Change in ventricular size with or without intervention10,12
- Change in an intraparenchymal hematoma9
- Change in extra-axial collection12
- Change in the imaging appearance of infarct1
- To follow or confirm stability13
- Mass effect and potential for midline shift14
- Change post-thrombectomy15
The Swoop system in intensive care units.
Learn More
1. Kuoy E, Glavis-Bloom J, Hovis G, et al. Point-of-Care Brain MRI: Preliminary Results from a Single-Center Retrospective Study [published online ahead of print, 2022 Aug 2]. Radiology. 2022;211721. doi:10.1148/radiol.211721
2. Sheth KN, Mazurek MH, Yuen MM, et al. Assessment of Brain Injury Using Portable, Low-Field Magnetic Resonance Imaging at the Bedside of Critically Ill Patients [published online ahead of print, 2020 Sep 8]. JAMA Neurol. 2020;78(1):41-47. doi:10.1001/jamaneurol.2020.3263
3. Jia L, Wang H, Gao Y, Liu H, Yu K. High incidence of adverse events during intra-hospital transport of critically ill patients and new related risk factors: a prospective, multicenter study in China. Crit Care. 2016;20:12. Published 2016 Jan 18. doi:10.1186/s13054-016-1183-y
4. Smith I, Fleming S, Cernaianu A. Mishaps during transport from the intensive care unit. Crit Care Med. 1990;18(3):278-281. doi:10.1097/00003246-199003000-00006
5. Martin M, Cook F, Lobo D, et al. Secondary Insults and Adverse Events During Intrahospital Transport of Severe Traumatic Brain-Injured Patients. Neurocrit Care. 2017;26(1):87-95. doi:10.1007/s12028-016-0291-5
6. Parmentier-Decrucq E, Poissy J, Favory R, et al. Adverse events during intrahospital transport of critically ill patients: incidence and risk factors. Ann Intensive Care. 2013;3(1):10. Published 2013 Apr 12. doi:10.1186/2110-5820-3-10
7. Beckmann U, Gillies DM, Berenholtz SM, Wu AW, Pronovost P. Incidents relating to the intra-hospital transfer of critically ill patients. An analysis of the reports submitted to the Australian Incident Monitoring Study in Intensive Care. Intensive Care Med. 2004;30(8):1579-1585. doi:10.1007/s00134-004-2177-9
8. Mello M, Studdert D, Thomas E, Yoon C, Brennan, T. Who Pays for Medical Errors? An Analysis of Adverse Event Costs, the Medical Liability System, and Incentives for Patient Safety Improvement. Journal of Empirical Legal Studies. 2007;4:835-860. doi:/10.1111/j.1740-1461.2007.00108.x
9. Mazurek MH, Cahn BA, Yuen MM, et al. Portable, bedside, low-field magnetic resonance imaging for evaluation of intracerebral hemorrhage. Nat Commun. 2021;12(1):5119. Published 2021 Aug 25. doi:10.1038/s41467-021-25441-6
10. Beekman R, Crawford A, Mazurek MH, et al. Bedside monitoring of hypoxic ischemic brain injury using low-field, portable brain magnetic resonance imaging after cardiac arrest. Resuscitation. 2022;176:150-158. doi:10.1016/j.resuscitation.2022.05.002
11. Kuoy E, Glavis-Bloom J, Hovis G, et al. Point-of-Care Brain MRI: Preliminary Results from a Single-Center Retrospective Study [published online ahead of print, 2022 Aug 2]. Radiology. 2022;211721. doi:10.1148/radiol.211721
12. Sien ME, Robinson AL, Hu HH, et al. Feasibility of and experience using a portable MRI scanner in the neonatal intensive care unit [published online ahead of print, 2022 Jul 4]. Arch Dis Child Fetal Neonatal Ed. 2022;fetalneonatal-2022-324200. doi:10.1136/archdischild-2022-324200
13. Yuen MM, Prabhat AM, Mazurek MH, et al. Portable, low-field magnetic resonance imaging enables highly accessible and dynamic bedside evaluation of ischemic stroke. Sci Adv. 2022;8(16):eabm3952. doi:10.1126/sciadv.abm3952
14. Sheth KN, Yuen MM, Mazurek MH, et al. Bedside detection of intracranial midline shift using portable magnetic resonance imaging. Sci Rep. 2022;12(1):67. Published 2022 Jan 7. doi:10.1038/s41598-021-03892-7
15. Sujijantarat N, Koo AB, Jambor I, et al. Low‐Field Portable Magnetic Resonance Imaging for Post‐Thrombectomy Assessment of Ongoing Brain Injury. Stroke. 2023;3:e000921. Published 2023 Jul 24. doi:10.1161/SVIN.123.000921
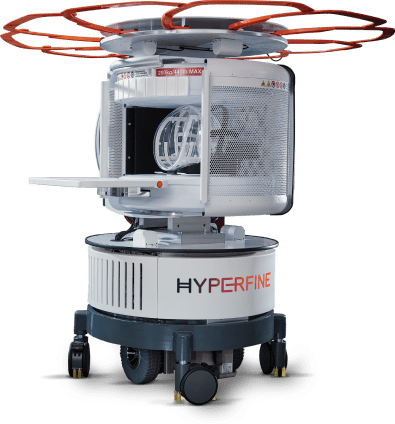
The Swoop® system brings MR brain imaging within reach.
The Swoop system brings brain imaging within reach for clinicians to help them make clinical decisions in a variety of healthcare settings across a range of conditions. The first FDA-cleared portable MR brain imaging system that combines safe, ultra-low-field magnetic resonance with proprietary artificial intelligence, the Swoop system potentially enables timelier treatment decisions, quicker discharges, and more efficient use of staff and hospital resources.